Placenta, types of placentas, placental barrier. What is the placental barrier? What is placental abruption
Species features of the fetal maternal placenta, umbilical cord. What is the placental barrier?
The placenta is a complex of tissue formations that develop from the choroid of the fetus and the mucous membrane of the uterus to connect the fetus with the maternal body and ensure metabolism between them. The placenta has two parts: fetal (choroid of the fetus) and maternal (mucous lining of the uterus).
The placenta is a unique formation that simultaneously performs the functions of the lungs, intestines, kidneys and endocrine glands. The placenta contains biological mechanisms that facilitate the transfer from mother to fetus of various substances necessary for its development: oxygen, nutrients, water, electrolytes, vitamins, antibodies. The fetus transfers carbon dioxide and substances to the mother - metabolic products. The placenta produces hormones (gonadotropins, prostaglandins, estrogens and progesterone) and activates the activity of enzymes. It contains vitamins (A, C, D) and many enzymes, under the influence of which carbohydrates, proteins and fats are broken down, after which they can pass through the placental barrier and be absorbed by fetal tissues.
The structure and structure of the fetal and uterine parts of the placenta in animals varies significantly.
In mares, donkeys, camels and pigs, the placenta, by the nature of the arrangement of villi and crypts, is diffuse or scattered, and by the characteristics of the connection between the fetal part of the placenta and the uterine placenta, it is epitheliochorionic. In a mare, the chorion resembles a cast of the inner surface of the pregnant uterus (Figure 2). The outer surface of the chorion is velvety, evenly covered with short hairs 1.5...2 mm long, growing into the crypts (recesses) of the uterine mucosa. The villus consists of a single layer of epithelium and a connective base containing one arterial and one venous capillary. Crypts are protrusions of single-layer epithelium into the thickness of the uterine mucosa.
Figure 2
Diagram of the location of the membranes in a horse fetus:
1 - fruit; 2 - amnion; 3 - allantois; 4 - chorion; 5 - urachus; 6 - uterine mucosa (maternal placenta)
The connection between the fetal and uterine parts of the placenta in these animals is weak, so during childbirth the placenta is easily and quickly separated without damaging the uterine mucosa and blood vessels. In this regard, the uterine part of the placenta of mares, donkeys, camels and pigs is classified as non-absorbing.
In cows, sheep and goats, the choroid has the shape of a bicornuate sac that fills the right and left horns of the uterus. On the outer surface of the fetal choroid, in contact with the uterine parts of the placenta (caruncles), fetal placentas (cotyledons) develop. In the caruncles there are depressions - crypts, into which the villi of the cotyledons enter, abundantly penetrated with blood capillaries. In areas where the choroid is not adjacent to the allantois, its surface is smooth, without villi.
Each caruncle connected to the cotyledon represents a separate placenta (Figure 2). In this regard, the placenta of cattle is called multiple: the number of placentas in cows, sheep and goats is 80...100. The caruncles of cows have a convex surface, while those of sheep and goats have a concave surface. During pregnancy, caruncles in cows reach the size of a chicken egg or more, standing out on the surface of the uterine mucosa in the form of mushroom-shaped formations sitting on a stalk. The caruncles of the fetal receptacle horn are larger in size compared to the caruncles of the uterine horn free from the fetus.
The placenta of ruminants, by the nature of the connection between the villi of the fetal part of the placenta and the crypts of the caruncles of the uterine mucosa, is classified as connective tissue, or desmochorionic (Figure 3). This is explained by the fact that the villi, plunging deeply into the crypts of the caruncles of the uterine mucosa, are in close contact with their connective tissue due to the destruction of its epithelial cover by the proteolytic enzyme of trophoblast.
Figure 3
Diagram of the location of the membranes in a cow fetus:
1 - fruit; 2 - amniotic fluid; 3 - amnion; 4 - allantois; 5 - urinary cavity; 6 - chorion; 7 - cotyledons; 8 - placental arteries; 9 - placental veins; 10 - umbilical artery; 11 -- umbilical vein; 12 - part of the amniotic sac from the free horn

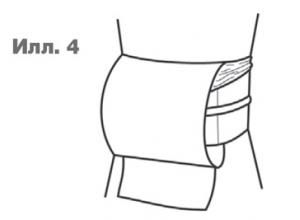
Figure 4
Uterine and fetal parts of the cow placenta:
1 - wall of the uterus; 2 - caruncle crypts; 3 - chorion; 4 - blood vessels of the chorion; 5 - fetal part of the placenta - cotyledon

In bitches and cats, the chorion has an oval shape, its villi are located only in the middle part in the form of a belt 2.5...6 cm wide, encircling the amniotic sac; the placenta of these animals is called zonal. Unlike other animal species, chorionic villi in carnivores grow deeply into the uterine mucosa (Figure 5). Under the influence of the enzyme they produce, the mucous membrane of the uterus melts, as a result of which the villi are directly adjacent to the endothelium of its vessels. On this basis, the placenta of bitches and cats is classified as endotheliochorial and at the same time as abscissing, since during childbirth there is a partial rejection of the uterine part of the placenta, accompanied by rupture of its vessels and bleeding. In bitches, the amniotic membranes and fluids are colored greenish-brown due to the presence of the pigment biliverdin.
Figure 5
Scheme of placental communication in mammals:
I - epitheliochoral; II - desmochorial; III - endotheliochorionic; IV - hemochorial; 1 - epithelium of the uterine mucosa; 2 - crypt epithelium; 3 villous epithelium; 4 - villus vessels; 5 - vessels of the uterine mucosa; 6 - gaps

Based on the nature of nutrition, placentas are divided into histiotrophic and embryotrophic. The histiotrophic placenta is characterized by the fact that nutrients resulting from the liquefaction and dissolution of tissue by chorionic enzymes are absorbed through its fetal part. Such a placenta is found in primates, rodents and carnivores.
Embryotrophic placenta in monohoofed animals, ruminants and omnivores. It received this name because the uterine part of the placenta produces a specific secretion - embryotroph ("royal jelly"). From the embryotroph, nutrients, after exposure to enzymes, penetrate through the chorion into the blood of the fetus.
Umbilical cord (umbilical cord). The umbilical cord has the form of a cord consisting of an outer shell, two umbilical arteries, one or two (in ruminants) veins, a urachus and a remnant of the yolk vesicle. The space between them is filled with embryonic tissue, called Warton's jelly, containing polysaccharide compounds of various origins and chemical natures. The accumulation of these substances in embryonic tissue - Wharton's jelly - increases in certain pathological conditions of the mother's body, which is regarded as a kind of protective biological barrier that prevents the spread of an infectious disease from mother to fetus.
The umbilical cord consists of a central and peripheral section. The central section is immersed in the aqueous membrane, and the peripheral section begins from the amniotic membrane and ends in the choroid.
In foals, the length of the umbilical cord is 70...100 cm. The umbilical vessels are firmly fused with the abdominal wall, as a result of which they break off outside the abdominal cavity or at the umbilical ring during childbirth.
In calves, the umbilical cord length is 30...40 cm. The umbilical arteries do not adhere to the umbilical ring, so their rupture during childbirth can occur in the abdominal cavity of the fetus. If the arteries in the umbilical cord vagina rupture, they are pulled into the abdominal cavity. The umbilical vein, due to its strong attachment to the umbilical ring, remains in the umbilical cord stump even after rupture.
In lambs and kids, the umbilical cord length is 7...12 cm, and in piglets 20...77 cm. The umbilical cord includes one vein and two arteries. At the end of pregnancy, the umbilical cord vessels twist and make up to eight turns.
In carnivorous animals, the length of the umbilical cord varies depending on the species and breed of the animal: on average it is 6... 10 cm. The umbilical cord has two arteries and two veins that merge in the umbilical ring. In bitches, the umbilical cord is very strong and does not break during childbirth under the influence of the weight of the fetus. The mother usually snacks on it.
The umbilical cord in animals of all species is innervated by the parasympathetic and sympathetic nervous systems. This confirms the possibility of impulse transmission from the fetus through the umbilical cord and the mother’s placenta.
And a number of other groups of animals, allowing for the transfer of material between the circulatory systems of the fetus and mother;
In mammals, the placenta is formed from the embryonic membranes of the fetus (villous, chorion, and urinary sac - allantois ( allantois)), which fit tightly to the wall of the uterus, form outgrowths (villi) protruding into the mucous membrane, and thus establish a close connection between the embryo and the maternal body, which serves for the nutrition and respiration of the embryo. The main purpose of the placenta is to ensure metabolism between mother and fetus. The placenta is permeable to low molecular weight substances, such as monosaccharides, water-soluble vitamins, and some proteins. Vitamin A is absorbed through the placenta in the form of its precursor, carotene. Under the action of enzymes, the following high-molecular substances are broken down in the placenta: proteins - into amino acids, fats - into fatty acids and glycerol, glycogen - into monosaccharides. The umbilical cord connects the embryo to the placenta.
The placenta together with the membranes of the fetus (the so-called afterbirth) in a woman comes out of the genital tract 5-60 minutes (depending on the tactics of labor) after the birth of the child.
Placentation
Structure of the placenta
The placenta is most often formed in the mucous membrane of the posterior wall of the uterus from the endometrium and cytotrophoblast. Layers of the placenta (from the uterus to the fetus - histologically):
- Decidua - transformed endometrium (with decidua cells rich in glycogen),
- Rohr's fibrinoid (Lanthans layer),
- Trophoblast, covering the lacunae and growing into the walls of the spiral arteries, preventing their contraction,
- Gaps filled with blood
- Syncytiotrophoblast (multinuclear symplast covering the cytotrophoblast),
- Cytotrophoblast (individual cells that form syncytium and secrete BAS),
- Stroma (connective tissue containing vessels, Kashchenko-Hoffbauer cells - macrophages),
- Amnion (on the placenta synthesizes more amniotic fluid, extraplacental - adsorbs).
Between the fetal and maternal parts of the placenta - the basal decidua - there are depressions filled with maternal blood. This part of the placenta is divided by decidual septa into 15-20 cup-shaped spaces (cotyledons). Each cotyledon contains a main branch consisting of the umbilical blood vessels of the fetus, which branches further into the many chorionic villi that form the surface of the cotyledon (labeled in the figure as Villus). Thanks to the placental barrier, the blood flow of the mother and fetus does not communicate with each other. The exchange of materials occurs by diffusion, osmosis or active transport. From the 3rd week of pregnancy, when the baby's heart begins to beat, the fetus is supplied with oxygen and nutrients through the “placenta”. Until 12 weeks of pregnancy, this formation does not have a clear structure; up to 6 weeks, it is located around the entire fetal egg and is called chorion; “placentation” takes place in 3-6 weeks.
Functions
The placenta forms blood-placental barrier, which is morphologically represented by a layer of fetal vascular endothelial cells, their basement membrane, a layer of loose pericapillary connective tissue, a trophoblast basement membrane, layers of cytotrophoblast and syncytiotrophoblast. The fetal vessels, branching in the placenta to the smallest capillaries, form (together with supporting tissues) chorionic villi, which are immersed in lacunae filled with maternal blood. It determines the following functions of the placenta.
Gas exchange
Oxygen from the mother’s blood penetrates into the fetal blood according to simple diffusion laws, and carbon dioxide is transported in the opposite direction.
Trophic and excretory
Through the placenta, the fetus receives water, electrolytes, nutrients and minerals, and vitamins; the placenta is also involved in the removal of metabolites (urea, creatine, creatinine) through active and passive transport;
Hormonal
The placenta plays the role of an endocrine gland: it produces chorionic gonadotropin, which supports the functional activity of the placenta and stimulates the production of large quantities of progesterone by the corpus luteum; placental lactogen, which plays an important role in the maturation and development of the mammary glands during pregnancy and in their preparation for lactation; prolactin, responsible for lactation; progesterone, which stimulates endometrial growth and prevents the release of new eggs; estrogens, which cause endometrial hypertrophy. In addition, the placenta is capable of secreting testosterone, serotonin, relaxin and other hormones.
Protective
The placenta has immune properties - it allows maternal antibodies to pass to the fetus, thereby providing immunological protection. Some antibodies pass through the placenta, providing protection to the fetus. The placenta plays a role in the regulation and development of the maternal and fetal immune systems. At the same time, it prevents the occurrence of an immune conflict between the organisms of the mother and the child - the mother’s immune cells, recognizing a foreign object, could cause rejection of the fetus. Syncytium absorbs certain substances circulating in the maternal blood and prevents them from entering the fetal blood. However, the placenta does not protect the fetus from certain narcotic substances and medications; they eat their afterbirth immediately after licking the newborn. They do this not only to eliminate the smell of blood that attracts predators, but also to provide themselves with the vitamins and nutrients they need after giving birth.
Notes
Literature
- Gavorka E. Human placenta, 1970.
- Milovanov A.P. Pathology of the mother-placenta-fetus system: A guide for doctors. - Moscow: “Medicine”. 1999 - 448 p.
- Tissue therapy. Under. ed. acad. USSR Academy of Medical Sciences N. A. Puchkovskaya. Kyiv, “Health”, 1975, 208 p.
- Filatov V.P. Tissue therapy (the doctrine of biogenic stimulants).
- Transcript of public lectures given to doctors at the Society's Central Lecture Hall in Moscow (third edition, expanded). - M.: Knowledge, 1955. - 63 p.
- Tsirelnikov N.I. Histophysiology of the placenta, 1981.
- Shirshev S. V. Mechanisms of immune control of reproductive processes. Ekaterinburg: Publishing House of the Ural Branch of the Russian Academy of Sciences, 1999. 381 p.
- Sapin M.R., Bilich G.L. Human anatomy: textbook in 3 volumes - ed. 3rd amendment, add. - M.: GEOTAR-Media, 2009. - T. 2. - 496 p.
1. Structure of the placenta. Surfaces of the placenta. Microscopic structure of mature placental villi.
2. Uterine-placental circulation.
3. Features of blood circulation in the mother-placenta-fetus system.
4. Basic functions of the placenta.
5. Respiratory function of the placenta. Trophic function of the placenta.
6. Endocrine function of the placenta. Placental lactogen. Chorionic gonodotropin (hCG, hCG). Prolactin. Progesterone.
7. Immune system of the placenta. Barrier function of the placenta.
8. Amniotic fluid. Volume of amniotic fluid. The amount of amniotic fluid. Functions of amniotic fluid.
9. Umbilical cord and after. Umbilical cord (umbilical cord). Options for attaching the umbilical cord to the placenta. Umbilical cord sizes.
Immune system of the placenta. Barrier function of the placenta.
Immune system of the placenta.
The placenta is a kind of immune barrier, separating two genetically foreign organisms (mother and fetus), therefore, during a physiological pregnancy, an immune conflict between the organisms of the mother and fetus does not arise. The absence of an immunological conflict between the organisms of the mother and fetus is due to the following mechanisms:
Absence or immaturity of the antigenic properties of the fetus;
- the presence of an immune barrier between mother and fetus (placenta);
- immunological characteristics of the mother’s body during pregnancy.
Barrier function of the placenta.
Concept " placental barrier"includes the following histological formations: syncytiotrophoblast, cytotrophoblast, a layer of mesenchymal cells (villous stroma) and the endothelium of the fetal capillary. The placental barrier can to some extent be likened to the blood-brain barrier, which regulates the penetration of various substances from the blood into the cerebrospinal fluid. However, in contrast from the blood-brain barrier, the selective permeability of which is characterized by the passage of various substances in only one direction (blood - cerebrospinal fluid), placental barrier regulates the transition of substances in the opposite direction, i.e. from fetus to mother. The transplacental transition of substances that are constantly in the mother’s blood and that enter it accidentally obeys different laws. The transition from mother to fetus of chemical compounds that are constantly present in the mother’s blood (oxygen, proteins, lipids, carbohydrates, vitamins, microelements, etc.) is regulated by fairly precise mechanisms, as a result of which some substances are contained in the mother’s blood in higher concentrations than in the blood of the fetus, and vice versa. In relation to substances that accidentally enter the maternal body (chemical production agents, medications, etc.), the barrier functions of the placenta are expressed to a much lesser extent.
Placental permeability is variable. During physiological pregnancy, the permeability of the placental barrier progressively increases until the 32-35th week of pregnancy, and then decreases slightly. This is due to the structural features of the placenta at different stages of pregnancy, as well as the needs of the fetus for certain chemical compounds.

Limited barrier functions placenta in relation to chemical substances that accidentally enter the mother’s body are manifested in the fact that toxic chemical products, most medications, nicotine, alcohol, pesticides, infectious agents, etc. pass through the placenta relatively easily. This poses a real risk of adverse effects of these agents on the embryo and fetus.
Barrier functions of the placenta are most fully manifested only in physiological conditions, i.e. during uncomplicated pregnancy. Under the influence of pathogenic factors (microorganisms and their toxins, sensitization of the mother’s body, the effects of alcohol, nicotine, drugs), the barrier function of the placenta is disrupted, and it becomes permeable even to substances that, under normal physiological conditions, pass through it in limited quantities.
From the very beginning of pregnancy until its end, it forms and functions mother-placenta-fetus system. The most important component of this system is placenta, which is a complex organ in the formation of which derivatives take part trophoblast and embryoblast, and decidual tissue. The function of the placenta is primarily aimed at providing sufficient conditions for the physiological course of pregnancy and normal development of the fetus. These functions include: respiratory, nutritional, excretory, protective, endocrine. All metabolic, hormonal, and immune processes during pregnancy are provided through vascular system of mother and fetus. Despite the fact that the blood of mother and fetus does not mix, since their divides the placental barrier, the fetus receives all the necessary nutrients and oxygen from the mother’s blood. The main structural component of the placenta is villous tree.
With the normal development of pregnancy, there is a relationship between the growth of the fetus, its body weight and the size, thickness, and weight of the placenta. Until 16 weeks of pregnancy, the development of the placenta is faster than the growth rate of the fetus. In case of death embryo (fetus) growth and development are inhibited chorionic villi and progression of involution-dystrophic processes in the placenta. Having reached the required maturity at 38-40 weeks of pregnancy, the processes of formation of new vessels and villi in the placenta stop.
1 - umbilical cord arteries
2 - stem fiber
3 - decidual septum
4 - decidual layer
5 - myometrium
6 - veins
7 - spiral arteries
8 - chorion
9 - amnion
10 - intervillous space
11 - umbilical cord vein
12 - cotyledon
The mature placenta is a disc-shaped structure with a diameter of 15-20 cm and a thickness of 2.5 - 3.5 cm. Its weight reaches 500-600 g. Maternal surface of the placenta, which faces the uterine wall, has a rough surface formed by the structures of the basal part of the decidua. Fetal surface of the placenta, which faces the fetus, is covered amniotic membrane. Below it are visible vessels that go from the place of attachment of the umbilical cord to the edge of the placenta. The structure of the fetal part of the placenta is represented by numerous chorionic villi, which are combined into structural formations - cotyledons. Each cotyledon is formed by a stem villus with branches containing fetal vessels. The central part of the cotyledon forms a cavity, which is surrounded by many villi. In a mature placenta there are from 30 to 50 cotyledons. The cotyledon of the placenta is conditionally comparable to a tree, in which the supporting villi of the first order are its trunk, villi of the second and third orders are large and small branches, intermediate villi are small branches, and terminal villi are leaves. The cotyledons are separated from each other by partitions (septa) emanating from the basal plate.
Intervillous space on the fetal side it is formed by the chorionic plate and the villi attached to it, and on the maternal side it is limited by the basal plate, the decidua and the partitions (septa) extending from it. Most placental villi are freely immersed in the intervillous space and washed with mother's blood. There are also anchor villi, which are fixed to the basal decidua and ensure attachment of the placenta to the wall of the uterus.

1 - superior vena cava
2 - oval hole
3 - inferior vena cava
4 - venous duct
5 - portal sinus
6 -
7 - umbilical cord vein
8 - umbilical cord arteries
9 - placenta
10 - epigastric arteries
11 - ductus arteriosus
Spiral arteries, which are the terminal branches of the uterine and ovarian arteries, nourishing the pregnant uterus, open into the intervillous space with 120-150 orifices, providing a constant flow of oxygen-rich maternal blood into the intervillous space. Due to pressure difference, which is higher in the maternal arterial bed compared to the intervillous space, oxygenated blood, from the mouths of the spiral arteries it is directed through the center of the cotyledon to the villi, washing them, reaches the chorionic plate and by dividing septa returns to the maternal bloodstream through the venous ostia. In this case, the blood flow of the mother and fetus is separated from each other. Those. maternal and fetal blood do not mix between themselves.
Transfer of blood gases, nutrients, metabolic products and other substances from maternal blood to fetal blood and vice versa is carried out at the moment of contact of the villi with the mother’s blood through the placental barrier. It is formed by the outer epithelial layer of the villus, the stroma of the villus and the wall of the blood capillary located inside each villus. Fetal blood flows through this capillary. Thus saturated with oxygen, the fetal blood from the capillaries of the villi is collected in larger vessels, which ultimately combine into umbilical vein, according to which oxygenated blood flows to the fetus. Having donated oxygen and nutrients to the fetus, blood, depleted of oxygen and rich in carbon dioxide, flows from the fetus through two arteries of the umbilical cord to the placenta, where these vessels are divided radially according to the number of cotyledons. As a result of further branching of the vessels inside the cotyledons, the fetal blood again enters the capillaries of the villi and is again saturated with oxygen, and the cycle repeats. Due to the passage of blood gases and nutrients through the placental barrier, the respiratory, nutritional and excretory functions of the placenta are realized. At the same time, oxygen enters the fetal bloodstream and carbon dioxide and other metabolic products of the fetus are excreted. At the same time, proteins, lipids, carbohydrates, microelements, vitamins, enzymes and much more are transported towards the fetus.

1 - endothelium of capillaries of terminal villi
2 - villus capillary
3 - villous stroma
4 - epithelial cover of villi
The placenta carries out important protective (barrier function) through the placental barrier, which has selective permeability in two directions. During the normal course of pregnancy, the permeability of the placental barrier increases until 32-34 weeks of pregnancy, after which it decreases in a certain way. However, unfortunately, quite a large number of medications, nicotine, alcohol, narcotic substances, pesticides, other toxic chemicals, as well as a number of pathogens of infectious diseases relatively easily penetrate through the placental barrier into the fetal bloodstream, which has an adverse effect on the fetus. In addition, under the influence of pathogenic factors, the barrier function of the placenta is disrupted to an even greater extent.
The placenta is anatomically and functionally connected to amnion (water membrane), which surrounds the fruit. The amnion is a thin membrane, which lines the surface of the placenta facing the fetus, passes to umbilical cord and merges with the skin of the fetus in the area of the umbilical ring. The amnion actively participates in the exchange amniotic fluid, in a number of metabolic processes, and also performs a protective function.
Connects the placenta and the fetus umbilical cord, which is a cord-like formation. Umbilical cord contains two arteries and one vein. The two arteries of the umbilical cord carry oxygen-depleted blood from the fetus to the placenta. Oxygenated blood flows through the umbilical cord vein to the fetus. The vessels of the umbilical cord are surrounded by a gelatinous substance called "Wharton's jelly". This substance provides elasticity to the umbilical cord, protects blood vessels and provides nutrition to the vascular wall. The umbilical cord can be attached (most often) in the center of the placenta and less often at the side of the umbilical cord or to the membranes. The length of the umbilical cord during a full-term pregnancy is on average about 50 cm.
The placenta, membranes and umbilical cord together form afterbirth, which is expelled from the uterus after the birth of the child.
The placental barrier refers to the selective properties of the placenta, as a result of which some substances penetrate from the mother’s blood into the blood of the fetus, while others are retained or enter the fetal body after appropriate biochemical processing.
The barrier separating the blood of the mother and the fetus in the intervillous space consists of the trophoblast epithelium, or syncytium, covering the villi, the connective tissue of the villi and the endothelium of their capillaries.
The barrier function of the placenta can only be performed under physiological conditions. The permeability of the placental barrier to harmful substances and microbes increases with pathological changes in the placenta resulting from damage to the villi by microbes and their toxins. Placental permeability may also increase due to thinning of the syncytium with increasing gestational age.
The exchange of gases (oxygen, etc.), as well as true solutions through the placental membrane, occurs according to the laws of osmosis and diffusion. This is facilitated by the difference in partial pressure in the blood of the mother and fetus. Proteins, fats, carbohydrates and other substances penetrate the placental barrier in the form of simple compounds formed under the influence of the enzymatic function of the placenta.
Different concentrations of potassium, sodium, phosphorus and other substances are created in the blood of the mother and fetus. Mother's blood, compared to fetal blood, is richer in proteins, neutral fats and glucose.
The fetal blood contains more protein-free nitrogen, free amino acids, potassium, calcium, inorganic phosphorus and other substances.
The placental barrier only partially protects the fetus from the penetration of harmful substances. Drugs, alcohol, nicotine, potassium cyanide, sulfonamides, quinine, mercury, arsenic, potassium iodide, antibiotics (penicillin and streptomycin), vitamins and hormones can pass through the placenta.
The penetration of substances from maternal blood into fetal blood is greatly influenced by the size of the molecules. During physiological pregnancy, substances with a molecular weight below 350 can penetrate through the placental barrier into the blood of the fetus. In pathologies of pregnancy (toxicosis, ionizing radiation, etc.), as a result of dysfunction of the placental barrier, high-molecular substances (antigens, antibodies, viruses) can penetrate into the blood of the fetus , toxins, bacteria, protozoa and helminths).
More on the topic Placental barrier:
- Placental barrier in anesthesiological terms. Pharmacokinetics and pharmacodynamics of drugs used in obstetric anesthesiology
- Placental insufficiency and toxicosis of pregnant women. Disorders of uteroplacental and placental-fetal circulation
Latest site materials
Health

Marshmallow cosmetic bag, crocheted Cosmetic bag, crocheted pattern for beginners
The cosmetic bag has long and permanently settled in the handbags of modern women, because makeup has to be corrected quite often during the day, and all cosmetics should be folded compactly and always be at hand. However, as a rule, all cosmetic bags are of the same type, and
Health
DIY Japanese kimono: pattern, job description How to make a Japanese kimono with your own hands
The Japanese word "kimono" literally means "clothing". A kimono traditionally means a complete set of clothing, including underwear, socks and shoes. In the West, kimono means a traditional Japanese costume with wide sleeves and no closure. Kimono length
Cosmetology

The best homemade masks for split ends Mask for split hair
Female attractiveness implies having well-groomed and shiny hair. This cannot be achieved if the curls become split. Often the tips suffer from this defect, but the entire length is often affected. Keratin will help correct the problem
Horoscope

Photos straight, round, ascending, descending, thin, houselike
Any specialist will tell you that eyebrows are the part of your face that creates its style, tone, and features. Their shape can actually say a lot about a person. Think about it, when we show certain emotions, our face involuntarily
Cooking
Dior who is the designer. Christian Dior. Fashion House of Dior: opening and work under the leadership of Christian Dior
Every time we pronounce the name Christian Dior, we mean style, sophistication and luxury of everything that this legendary brand with more than half a century of history produces - clothes, perfumes, cosmetics. Even as a child, a gypsy predicted the future great couturier
Cooking

Artistic painting of nails How to draw poppies - master class
From year to year, nail design and artistic painting remain a trend for manicure. The amazing drawings that professionals create are simply amazing and mesmerizing. In addition, choosing this nail design means that your manicure will be absolutely unique.